
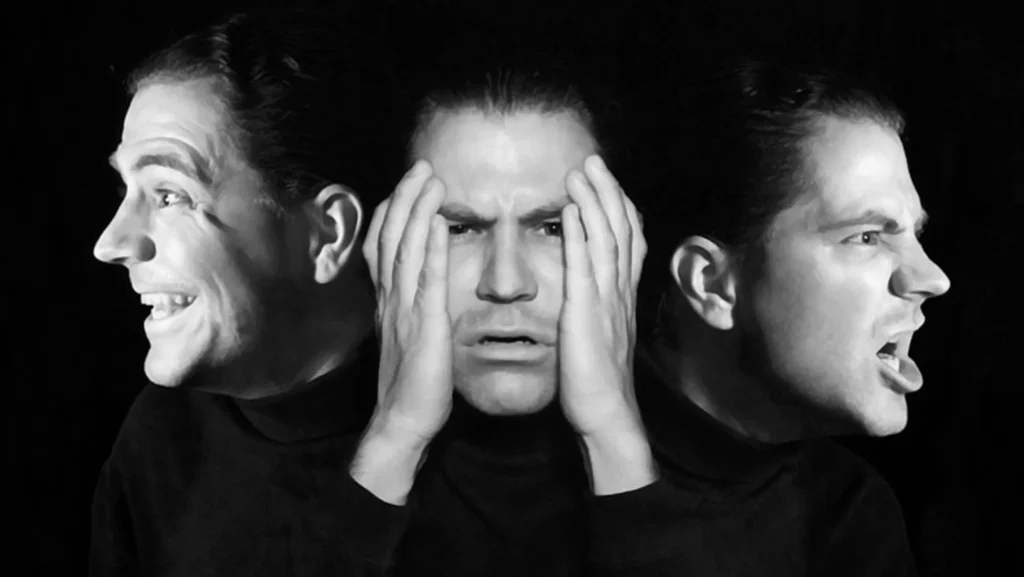
Bipolar Disorder is a mental health condition marked by extreme shifts in mood, energy, and activity levels. These mood episodes range from manic or hypomanic highs to depressive lows. The condition can significantly affect a person’s ability to carry out daily tasks, maintain relationships, and function in work or academic environments. It typically emerges in late adolescence or early adulthood, although it can develop at any age.
ADHD symptoms are grouped into two primary categories: inattention and hyperactivity/impulsivity. These symptoms must be chronic, pervasive, and inappropriate for the individual’s developmental level.
Diagnosing ADHD requires a comprehensive assessment that includes:
Bipolar disorder is a chronic condition that requires long-term management. Treatment is typically a combination of medication, psychotherapy, and lifestyle strategies.
Mood Stabilizers: Lithium is one of the most effective long-term treatments. Other mood stabilizers include valproate and lamotrigine.
Antipsychotics: Atypical antipsychotics (e.g., quetiapine, olanzapine) help manage manic or mixed episodes.
Antidepressants: Used cautiously and usually in combination with a mood stabilizer to prevent triggering mania.
Cognitive Behavioral Therapy (CBT): Helps patients recognize and manage thought patterns and behaviors.
Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on maintaining regular daily routines and sleep schedules.
Family-Focused Therapy: Educates family members about the condition and improves communication and support systems.
Sleep Hygiene: Consistent sleep patterns can help prevent mood episodes.
Stress Reduction: Mindfulness, yoga, and stress management techniques lower relapse risk.
Healthy Diet and Exercise: Promotes overall well-being and mood stability.
Avoidance of Substances: Alcohol and drugs can trigger or worsen mood episodes.
Development of a crisis plan in case of severe episodes.
Ongoing support from therapists, psychiatrists, and peer support groups.